Multi-Payer Reporting Suite
View Population Health Metrics Agnostic to Payer
View Population Health Metrics Agnostic to Payer

New Webinar
Check out the webinar on the new Prediction Tools below!
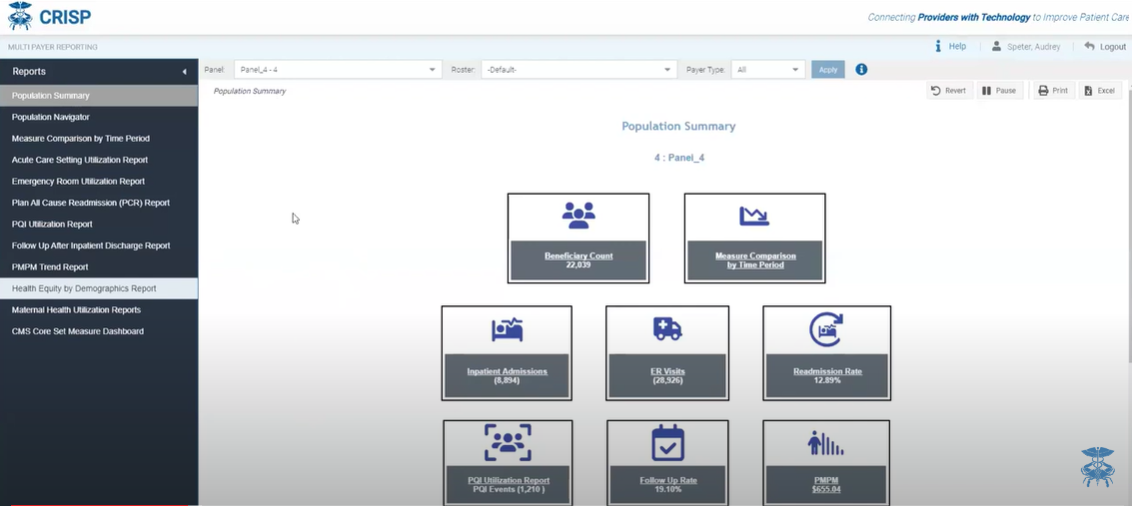
The Multi-payer Reporting Suite includes 8 top-level, Tableau-based reports populated using both Medicare and Medicaid claims data. The goal of the reporting suite is to allow users to view population-health metrics and access care management tools across their entire patient populations, agnostic to payer. The reporting suite provides population-level aggregate views, as well as beneficiary and claim-level details. A Population Navigator allows users to custom curate their own patient lists, within their CRISP patient panels to investigate sub-populations more easily.
The Multi-Payer Reporting Suite displays patients on an organization’s panel that are enrolled in Medicare FFS, Medicaid FFS, or Medicaid Managed Care.
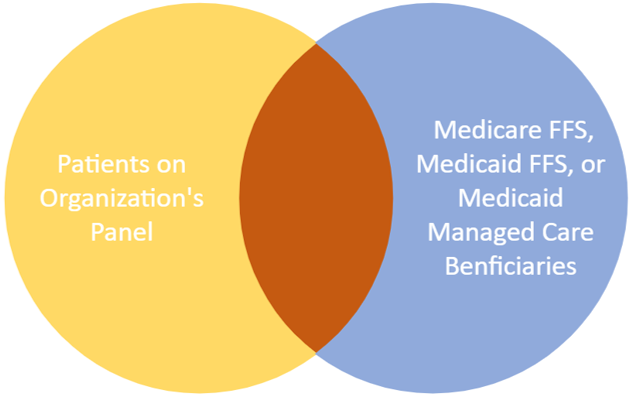
The suite only shows data for patients on an organization’s panel with the following coverage:
Administrative claims data includes all care settings and services covered under Medicare and Medicaid. Data displayed are for the last 36 months, with a two-month data lag. There is an additional 3-month lag for claim completeness (i.e., incomplete data are shown with a claim lag indicator)

Watch the CRISP Reporting Services team give an overview and demo of the Multi-Payer Reporting Suite. For the last couple of months, CRISP, in partnership with hMetrix, collaborated with Maryland Medicaid and the Maryland Primary Care Program (MDPCP) to create a reporting suite that 1.) Aligns efforts between Maryland Medicaid and MDPCP 2.) Provides users the opportunity to view Maryland Medicaid and Medicare data in one place. The suite displays the last three years of Medicare and Medicaid data for patients on an organization’s ENS panel submitted to CRISP. Within the suite, users can better understand trends in hospital utilization, facilitate care coordination, and monitor population health for their Medicare and Medicaid patients.

View a recording of the Multi-Payer Reporting Suite Showcase from the 2025 CRISP Annual Summit featuring speakers from CRISP, GBMC, and MD Medicaid.
Quality Dashboard Demo
Prediction Tools Demo
Subscribe