ALERT PORTAL USERS: Please navigate directly to portal.crisphealth.org if you are attempting to login into the CRISP Portal
View Topics & Resources
Explore Topics
Other Resources
EQIP Enrollment will be open from July 1st to August 29th
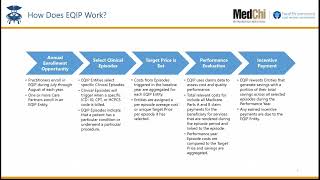
EQIP is a voluntary, Advanced Alternative Payment Model (AAPM) that engages practitioners who treat Maryland Medicare beneficiaries in care transformation and value-based payment through an episode-based approach. This Performance Year includes 123 episodes across a variety of clinical episode categories. Please find the list of PY5 episodes below under the Enrollment section.
EQIP Subpages
The Episode Quality Improvement Program (EQIP) is a voluntary program that will provide incentive payments to physicians who improve the quality of care and reduce the cost of care that they provide to Maryland Medicare patients. EQIP tests an approach that ties healthcare payments to the quality and cost of services provided under a clinical ‘episode’ for a set period. This includes relevant set of services delivered to a related to a medical condition, procedure or health care event during a defined time period.
Source and Additional Information: HSCRC and Medchi
EQIP Enrollment Timeline
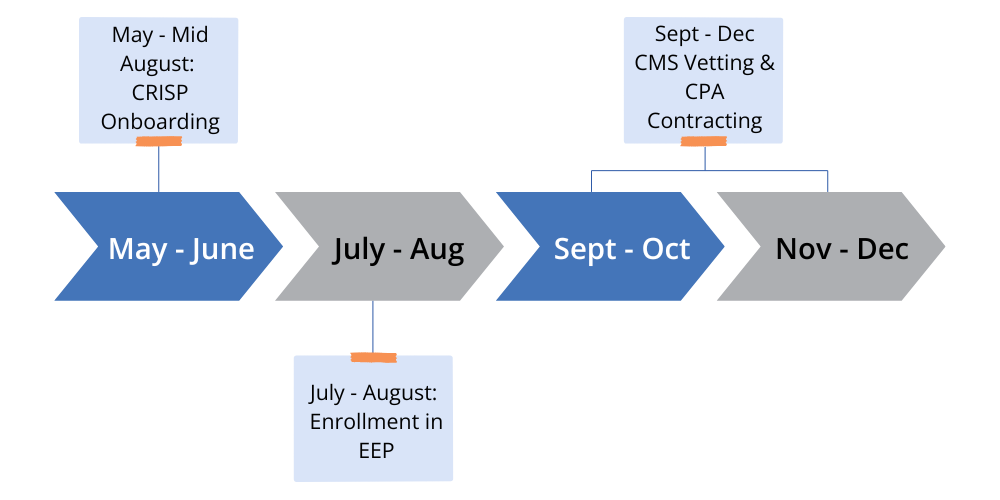
EQIP Enrollment for PY4 is closed. PY5 Enrollment will open July 2025
EQIP Eligible Episodes PY5 Slide Deck – This is a listing of all of the available episodes you could participate in for Performance Year 5.
EQIP Enrollment Webinar – This recording and slide deck reviews the steps to enroll in the EQIP Program for Performance Year 5.
EQIP Videos
EQIP Policy Resources and Documentation
Performance Year 5 (CY2026) – Enrollment Now Open
EQIP Introduction Policy Guide – PY5 – this document will cover the overarching goals of the program, the program structure and key policy components critical for participation
EQIP Specifications and Methodology PY5 – this document is a comprehensive reference on the methodology and implementation of the program
Performance Year 4 (CY2025)
EQIP Introduction Policy Guide – PY4 – this document will cover the overarching goals of the program, the program structure and key policy components critical for participation
EQIP Specifications and Methodology PY4 – this document is a comprehensive reference on the methodology and implementation of the program
EQIP Episode Playbook PY4 – this document is breakdown of all available episode and their corresponding definitions